Comorbiditeam
a compendium of my experiences being diagnosed with dissociative identity disorder, what I have learned and the language I use. It is a work in progress, constantly evolving, and probably always will be
this page and its sections are in black and white, except...
... buttons & links will turn yellow-green when hovered over
... links containing images (will be labeled as such)
+
+
+
Links to Detailed Definitions Not Yet Active
Dissociative Identity Disorder
Code: 6B64 | Description
Dissociative identity disorder is characterised by disruption of identity in which there are two or more distinct personality states (dissociative identities) associated with marked discontinuities in the sense of self and agency. Each personality state includes its own pattern of experiencing, perceiving, conceiving, and relating to self, the body, and the environment. At least two distinct personality states recurrently take executive control of the individual’s consciousness and functioning in interacting with others or with the environment, such as in the performance of specific aspects of daily life such as parenting, or work, or in response to specific situations (e.g., those that are perceived as threatening). Changes in personality state are accompanied by related alterations in sensation, perception, affect, cognition, memory, motor control, and behaviour. There are typically episodes of amnesia, which may be severe. The symptoms are not better explained by another mental, behavioural or neurodevelopmental disorder and are not due to the direct effects of a substance or medication on the central nervous system, including withdrawal effects, and are not due to a disease of the nervous system or a sleep-wake disorder. The symptoms result in significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
Diagnostic Requirements
Essential Features:
- Disruption of identity characterized by the presence of two or more distinct personality states (dissociative identities), involving marked discontinuities in the sense of self and agency. Each personality state includes its own pattern of experiencing, perceiving, conceiving, and relating to self, the body, and the environment.- At least two distinct personality states recurrently take executive control of the individual’s consciousness and functioning in interacting with others or with the environment, such as in the performance of specific aspects of daily life (e.g., parenting, work), or in response to specific situations (e.g., those that are perceived as threatening).- Changes in personality state are accompanied by related alterations in sensation, perception, affect, cognition, memory, motor control, and behaviour. There are typically episodes of amnesia inconsistent with ordinary forgetting, which may be severe.- The symptoms are not better accounted for by another mental disorder (e.g., Schizophrenia or Other Primary Psychotic Disorder).- The symptoms are not due to the effects of a substance or medication on the central nervous system, including withdrawal effects (e.g., blackouts or chaotic behaviour during substance intoxication), and are not due to a Disease of the Nervous System (e.g., complex partial seizures) or to a Sleep-Wake disorder (e.g., symptoms occur during hypnagogic or hypnopompic states).- The symptoms result in significant impairment in personal, family, social, educational, occupational or other important areas of functioning. If functioning is maintained, it is only through significant additional effort.
Additional Clinical Features:
- Alternation between distinct personality states is not always associated with amnesia. That is, one personality state may have awareness and recollection of the activities of another personality state during a particular episode. However, substantial episodes of amnesia are typically present at some point during the course of the disorder.- In individuals with Dissociative Identity Disorder, it is common for one personality state to be ‘intruded upon’ by aspects of other non-dominant, alternate personality states without their taking executive control, as in Partial Dissociative Identity Disorder. These intrusions may involve a range of features, including cognitive (intruding thoughts), affective (intruding affects such as fear, anger, or shame), perceptual (e.g., intruding voices or fleeting visual perceptions), sensory (e.g., intruding sensations such as being touched, pain, or altered perceived size of the body or of part of the body), motor (e.g., involuntary movements of an arm and hand), and behavioural (e.g., an action that lacks a sense of agency or ownership). The personality state that is intruded upon in this way commonly experiences the intrusions as aversive, and may or may not realize that the intrusions relate to features of other personality states.- Dissociative Identity Disorder is commonly associated with serious or chronic traumatic life events, including physical, sexual, or emotional abuse.
Boundary with Normality (Threshold):
- The presence of two or more distinct personality states does not always indicate the presence of a mental disorder. In certain circumstances (e.g., as experienced by ‘mediums’ or other culturally accepted spiritual practitioners) the presence of multiple personality states is not experienced as aversive and is not associated with impairment in functioning. A diagnosis of Dissociative Identity Disorder should not be assigned in these cases.
Course Features
- Onset of Dissociative Identity Disorder is most commonly associated with traumatic experiences, especially physical, sexual, and emotional abuse or childhood neglect. The onset of identity changes can also be triggered by removal from ongoing traumatizing circumstances, death or serious illness of the perpetrator of abuse, or by other unrelated traumatic experiences later in life.- Dissociative Identity Disorder usually has a recurrent and fluctuating clinical course.- Some individuals remain highly impaired in most aspects of functioning, despite treatment. Individuals with Dissociative Identity Disorder are at high risk for self-injurious behaviour and suicide attempts.- Although symptoms can spontaneously remit with age, recurrence may occur during periods of increased stress.- Recurrent or chronic ongoing traumatic experiences are associated with poorer prognosis.- Dissociative Identity Disorder often co-occurs with other mental disorders. In such cases, identity alternations can influence the symptom presentation of the co-occurring disorders.
Developmental Presentations:
- Onset of Dissociative Identity Disorder can occur across the lifespan. Initial identity changes usually appear at an early age, but dissociative identities are not typically fully developed. Instead, children present with discontinuities of experience and marked interference among mental states.- Identification of Dissociative Identity Disorder in children can be difficult because symptoms manifest in a variety of ways that overlap with other mental disorders, including those involving conduct problems, mood and anxiety symptoms, learning difficulties, and auditory hallucinations. Young children often project their dissociated identities onto toys or other objects, so that abnormalities in their identity may only become detectable as children age and their behaviours become less developmentally appropriate. With adequate treatment, children with Dissociative Identity Disorder tend to have a better prognosis than adults.- Early identity changes in adolescence characteristic of Dissociative Identity Disorder may be mistaken for developmentally typical difficulties with emotional and behavioural regulation.- Older patients with Dissociative Identity Disorder may present with what appears to be late-life onset paranoia or cognitive impairment, or atypical mood, psychotic or obsessive-compulsive symptoms.
Culture Related Features:
- Features of Dissociative Identity Disorder can be influenced by the individual’s cultural background. For example, individuals may present with dissociative symptoms of movement, behaviour, or cognition – such as non-epileptic seizures and convulsions, paralyses, or sensory loss – in socio-cultural settings where such symptoms are common. These symptoms typically remain persistent and debilitating until the underlying Dissociative Identity Disorder is identified and treated.- Acculturation or prolonged intercultural contact may shape the characteristics of the dissociative identities; for example, identities in India may speak English exclusively and wear Western clothes as a sign of their difference from the usual personality state.- In some societies, presentations of Dissociative Identity Disorder may occur after stressful exposures (e.g., recurrent parental affect dysregulation), which may or may not involve physical or sexual abuse. The tendency toward dissociative responses to stressors may be increased in cultures with less individualistic (‘bounded’) conceptions of the self or in circumstances of socioeconomic deprivation.
Sex- and/or Gender-Related Features:
- Prior to puberty, prevalence of Dissociative Identity Disorder does not appear to vary by gender. After puberty, prevalence appears to be higher in females.- Significant gender differences have been observed in the symptoms of Dissociative Identity Disorder across the lifespan. Females with Dissociative Identity Disorder often present with more dissociative identities and tend to experience more acute dissociative states (e.g., amnesia, conversion symptoms, self-mutilation) than males. Males with Dissociative Identity Disorder are more likely to deny their symptoms or exhibit violent or criminal behaviours.
Boundaries with Other Disorders and Conditions (Differential Diagnosis):
-Boundary with Trance Disorder and Possession Trance Disorder: Trance Disorder is not characterized by the presence of two or more distinct personality states. In Possession Trance Disorder, the individual’s customary sense of personal identity is replaced by an external ‘possessing’ identity, which is attributed to the influence of a spirit, power, deity or other spiritual entity. Behaviours or movements are experienced as being controlled by the possessing agent. Individuals who describe both internal distinct personality states that assume executive control as well as episodes of being controlled by an external possessing identity should receive a diagnosis of Dissociative Identity Disorder rather than Possession Trance Disorder.-Boundary with Partial Dissociative Identity Disorder: In Dissociative Identity Disorder, discontinuities in agency and sense of self are marked (manifested in episodes of executive control, often including amnesia, and greater elaboration of the personality states), whereas in Partial Dissociative Identity Disorder these discontinuities are less pronounced. In Partial Dissociative Identity Disorder, one personality state is dominant and functions in daily life (e.g., parenting, work), but is intruded upon by non-dominant personality states (dissociative intrusions). Unlike in Dissociative Identity Disorder, the non-dominant personality states do not recurrently take executive control of the individual’s consciousness and functioning to the extent that they perform in specific aspects of daily life (e.g., parenting, work). However, in Partial Dissociative Identity Disorder, there may be occasional, limited and transient episodes in which a distinct personality state assumes executive control to engage in circumscribed behaviours (e.g., in response to extreme emotional states, episodes of self-harm, or the reenactment of traumatic memories). In Partial Dissociative Identity Disorder, the non-dominant personality states are not elaborated to the extent observed in Dissociative Identity Disorder. For example, they may not be oriented to the present, may have the identity of a child, or may be mostly or exclusively involved in reenacting traumatic memories. In addition, there are typically (although not always) significant episodes of amnesia in Dissociative Identity Disorder, which may be severe. In contrast, episodes of amnesia in Partial Dissociative Identity Disorder, if present, are typically brief and restricted to extreme emotional states or episodes of self-harm.-Boundary with other Dissociative Disorders: Dissociative Identity Disorder is distinguished from other Dissociative Disorders by the presence of two distinct personality states that recurrently take executive control of the individual’s consciousness and functioning. This does not occur in any other dissociative disorder (except possibly for limited circumstances in Partial Dissociative Identity Disorder, as described above). An additional Dissociative Disorder diagnosis should not be assigned based on phenomena that occur in specific relationship to changes in personality states (e.g., memory loss, changes in motor or sensory functioning, experiences of depersonalization and derealization).-Boundary with Schizophrenia or Other Primary Psychotic Disorders: Individuals with Dissociative Identity Disorder may report experiencing symptoms such as hearing voices or intrusive thoughts that may also occur in Schizophrenia or Other Primary Psychotic Disorders. However, individuals with Dissociative Identity Disorder do not typically exhibit delusions, formal thought disorder, or negative symptoms (as in Schizophrenia or Schizoaffective Disorder) or rapid onset and rapidly fluctuating symptoms (as in Acute and Transient Psychotic Disorder). In the absence of other symptoms supporting a diagnosis of Schizophrenia or Other Primary Psychotic Disorder, intrusive phenomena such as hearing voices may suggest the presence of dissociative personality states.-Boundary with Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder: Individuals with Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder may experience alterations in identity and sense of agency during episodes of re-experiencing of traumatic events (e.g., during flashbacks). For example, they may feel that they are unable to control their experiences or reactions during the re-experiencing episode or that they are in a different time in their own lives. However, these episodes are not characterized by a distinct personality state taking executive control of the individual’s consciousness and functioning. Because Dissociative Identity Disorder is commonly associated with serious or chronic traumatic life events, it may co-occur with Post-Traumatic Stress Disorder or Complex Post-Traumatic Stress Disorder, and both diagnoses may be assigned if the full diagnostic requirements for both disorders are met.-Boundary with Obsessive-Compulsive Disorder: Obsessive-Compulsive Disorder involves repetitive and persistent thoughts (e.g., of contamination), images (e.g., of violent scenes), or impulses/urges (e.g., to stab someone) that are experienced as intrusive and unwanted (obsessions) as well as repetitive behaviours, including repetitive mental acts, that the individual feels driven to perform (compulsions). However, Obsessive-Compulsive Disorder is not characterized by discontinuities in the sense of self and agency or the presence of two or more distinct personality states.-Boundary with Personality Disorder: Personality Disorder, particularly with Borderline pattern, is characterized by persistent disturbances in sense of identity and self-direction, and often by problems with affect regulation. Personality Disorder does not involve the presence of two or more distinct personality states, but some individuals with Severe Personality Disorder exhibit transient dissociative experiences during times of stress or intense emotion.
Dissociative Identity Disorder
Diagnostic Criteria | F44.81
A. Disruption of identity characterized by two or more distinct personality states, which may be described in some cultures as an experience of possession. The disruption in identity involves marked discontinuity in sense of self and sense of agency, accompanied by related alterations in affect, behavior, consciousness, memory, perception, cognition,and/or sensory-motor functioning. These signs and symptoms may be observed by others or reported by the individual.B. Recurrent gaps in the recall of everyday events, important personal information, and/or traumatic events that are inconsistent with ordinary forgetting.C. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.D. The disturbance is not a normal part of a broadly accepted cultural or religious practice.
Note: In children, the symptoms are not better explained by imaginary playmates or other fantasy play.E. The symptoms are not attributable to the physiological effects of a substance (e.g., blackouts or chaotic behavior during alcohol intoxication) or another medical condition (e.g., complex partial seizures).
Diagnostic Features
The defining feature of dissociative identity disorder is the presence of two or more distinct personality states or an experience of possession (Criterion A). The overtness or covertness of these personality states varies as a function of psychological motivation, current level of stress, cultural context, internal conflicts and dynamics, and emotional resilience, among other factors. Sustained periods of identity confusion/alteration may occur when psychosocial pressures are severe and/or prolonged. In those cases of dissociative identity disorder that present as the individual being possessed by external identities (e.g., spirits, demons) (possession-form dissociative identity disorder), and in a small proportion of non-possession-form cases, manifestations of alternate identities are readily observable. Most individuals with non-possession-form dissociative identity disorder do not overtly display, or only subtly display, their discontinuity of identity, and only a minority present to clinical attention with discernible alternation of identities. The elaboration of dissociative personality states with different names, wardrobes, hairstyles, handwritings, accents, and so forth, occurs in only a minority of individuals with the non-possession-form dissociative identity disorder and is not essential to diagnosis. In those cases where alternate personality states cannot be directly observed, the presence of distinct personality states can be identified by sudden alterations or discontinuities in the individual’s sense of self and sense of agency (Criterion A), and recurrent dissociative amnesias (Criterion B).Criterion A symptoms are related to discontinuities of experience that can affect any aspect of an individual’s functioning. Individuals with dissociative identity disorder may report the feeling that they have suddenly become depersonalized observers of their own speech and actions, which they may feel powerless to stop (i.e., impaired sense of self and impaired sense of agency). These individuals may also report perceptions of voices (e.g., a child’s voice, voices commenting on the individual’s thoughts or behavior, persecutory voices and command hallucinations). In some cases, hearing voices is specifically denied, but the individual reports multiple, perplexing, independent thought streams over which the individual experiences no control. Individuals with dissociative identity disorder may report hallucinations in all sensory modalities: auditory, visual, tactile, olfactory, and gustatory.Strong emotions, impulses, thoughts, and even speech or other actions may suddenly materialize, without a sense of personal ownership or control (i.e., lack of sense of agency). Conversely, thoughts and emotions may unexpectedly vanish, and speech and actions are abruptly inhibited. These experiences are frequently reported as ego-dystonic and puzzling. Attitudes, outlooks, and personal preferences (e.g., about food, activities, gender identity) may suddenly shift. Individuals may report that their bodies feel different (e.g., like a small child, the opposite gender, different ages simultaneously). Alterations in sense of self and agency may be accompanied by a feeling that attitudes, emotions, and behaviors—even the individual’s own body—are “not mine” or are “not under my control.” Although most Criterion A symptoms are subjective, these sudden discontinuities in speech, affect, and behavior may be witnessed by family, friends, or the clinician.In most individuals with dissociative identity disorder, switching/shifting of states is subtle and may occur with only subtle changes in overt presentation. State switching may be more overt in the possession form of dissociative identity disorder. In general, the individual with dissociative identity disorder experiences himself or herself as multiple, simultaneously overlapping and interfering states.Dissociative amnesia (Criterion B) manifests in several major domains: 1) gaps in any aspect of autobiographical memory (e.g., important life events like getting married or giving birth, lack of recall of all school experiences before high school); 2) lapses in memory of recent events or well-learned skills (e.g., how to do one’s job, use a computer, cook or drive); and 3) discovery of possessions that the individual has no recollection of ever owning (e.g., clothing, weapons, tools, writings or drawings that he or she must have created). Dissociative fugues, with amnesia for travel, are common. Individuals may report suddenly finding themselves in another city, at work, or even at home: in the closet, under the bed, or running out of the house. Amnesia in individuals with dissociative identity disorder is not limited to stressful or traumatic events; it can involve everyday events as well. Individuals may report major gaps in ongoing memory (e.g., experiencing “time loss,” “blackouts,” or “coming to” in the midst of doing something). Dissociative amnesia may be apparent to others (e.g., the individual does not recall something others witnessed that he or she did or said, cannot remember his or her own name, or may fail to recognize spouse, children, or close friends). Minimization or rationalization of amnesia is common.Possession-form identities in dissociative identity disorder typically manifest behaviorally as if a “spirit,” supernatural being, or outside person has taken control, with the individual speaking or acting in a distinctly different manner. For example, an individual’s behavior may give the appearance that her identity has been replaced by the “ghost” of a girl who died by suicide in the same community years before, speaking and acting as though she were still alive. The identities that arise during possession-form dissociative identity disorder present recurrently, are unwanted and involuntary, and cause clinically significant distress or impairment (Criterion C). However, the majority of possession states that occur around the world are usually part of a broadly accepted cultural or religious practice and therefore do not meet criteria for dissociative identity disorder (Criterion D).
Associated Features
Individuals with dissociative identity disorder typically present with comorbid depression, anxiety, substance abuse, self-injury, or another common symptom. Nonepileptic seizures and other functional neurological symptoms are prominent in some presentations of dissociative identity disorder, especially in some non-Western settings. Some individuals, especially in Western settings, may present with apparently refractory neurological symptoms, such as headaches, seizures, or symptoms suggestive of multiple sclerosis.Individuals with dissociative identity disorder often conceal, or are not fully aware of, disruptions in consciousness, amnesia, or other dissociative symptoms. Many individuals with dissociative identity disorder report dissociative flashbacks during which they experience a sensory reliving of a previous event as though it were occurring in the present, often with a change of identity, a partial or complete loss of contact with or disorientation to current reality during the flashback, and a subsequent amnesia for the content of the flashback. Individuals with the disorder typically report multiple types of interpersonal maltreatment during childhood and adulthood. Other overwhelming early life events, such as multiple long, painful, early-life medical procedures, also may be reported. Nonsuicidal self-injury is frequent. On standardized measures, these individuals report higher levels of hypnotizability and dissociative symptoms compared with other clinical groups and healthy control subjects. Some individuals experience transient psychotic phenomena or episodes.Among personality features, avoidant personality features most often rate highest in individuals with dissociative identity disorder, and some individuals with dissociative identity disorder are so avoidant that they prefer to be alone. When decompensated, some individuals with dissociative identity disorder display features of borderline personality disorder (i.e., self-destructive high-risk behaviors, and mood instability). Many individuals with dissociative identity disorder display attachment problems but typically do not exhibit frantic activity to avoid being abandoned. Some have stable long-term relationships, albeit frequently dysfunctional and/or abusive ones, from which they may have difficulty extricating themselves. Obsessional personality features are common in dissociative identity disorder, more so than histrionic personality features. A subgroup of individuals with dissociative identity disorder have narcissistic and/or antisocial personality features.
Prevalence
The 12-month prevalence of dissociative identity disorder among adults in a small U.S. community study was 1.5%. Lifetime prevalence of dissociative identity disorder was 1.1% in a representative sample of community-based women in mid-eastern Turkey.
Development and Course
The disorder may first manifest at almost any age from early childhood to late life. Children usually do not present with identity shifting, instead presenting primarily with independently acting, imaginary companions, or as personified “mood” states (Criterion A phenomena). Dissociation in children may generate problems with memory, concentration, and attachment, and may be associated with traumatic play. In adolescents, dissociative identity disorder commonly comes to clinical attention because of externalizing symptoms, suicidal/self-destructive behavior, or rapid behavioral shifts often ascribed to other disorders such as attention- deficit/hyperactivity disorder or childhood bipolar disorder. Some children with dissociative identity disorder can also be quite aggressive and irritable. Older individuals with dissociative identity disorder may present with symptoms that appear to be late-life mood disorders, obsessive-compulsive disorder, paranoia, psychotic mood disorders, or even cognitive disorders attributable to dissociative amnesia.Overt identity alteration/confusion may be triggered by many factors, such as later traumatic experiences (e.g., sexual assault), or even seemingly inconsequential stressors, like a minor motor vehicle accident. The experience of other major or cumulative life stressors may also worsen symptoms, including life events such as the individual’s children reaching the same age at which the individual was significantly abused or traumatized. The death of, or the onset of a fatal illness in, the individual’s abuser(s) is another example of an event that may worsen symptoms. Individuals with dissociative identity disorder are at high risk for adult interpersonal trauma such as rape, intimate partner violence, and sexual exploitation, including ongoing incestuous abuse into adulthood, as well as adult trafficking.
Risk and Prognostic Factors
Environmental. In the context of family and attachment pathology, early life trauma (e.g., neglect and physical, sexual, and emotional abuse, usually before ages 5–6 years) represents a risk factor for dissociative identity disorder. In studies from diverse geographic regions, about 90% of the individuals with the disorder report multiple types of early neglect and childhood abuse, often extending into late adolescence. Some individuals report that maltreatment primarily occurred outside the family, in school, church, and/or neighborhoods, including being bullied severely. Other forms of repeated early-life traumatic experiences include multiple, painful childhood medical and surgical procedures; war; terrorism; or being trafficked beginning in childhood. Onset has also been described after prolonged and often transgenerational exposure to dysfunctional family dynamics (e.g., overcontrolling parenting, insecure attachment, emotional abuse) in the absence of clear neglect or sexual or physical abuse.Genetic and physiological. Twin studies suggest that genetics account for around 45%–50% of the interindividual variance in dissociative symptoms, with nonshared, stressful, and traumatic environmental experiences accounting for most of the additional variance. Several brain regions have been implicated in the pathophysiology of dissociative identity disorder, including the orbitofrontal cortex, hippocampus, parahippocampal gyrus, and amygdala.Course modifiers. Ongoing sexual, physical, and emotional trauma often leads to significant difficulties in later functioning. Poorer outcome in adults is commonly related to severe psychosocial stressors, revictimization, ongoing sexual or physical abuse or exploitation, intimate partner violence, refractory substance use, eating disorders, severe medical illness, enmeshment with the individual’s abusive family of origin, or ongoing involvement in criminal subgroups. Poorer functioning may also be related to perpetration of child maltreatment or intimate partner violence by individuals with dissociative identity disorder.
Culture-Related Diagnostic Issues
Many features of dissociative identity disorder can be influenced by the individual’s sociocultural background. In settings where possession symptoms are common (e.g., rural areas in low- and middle-income countries, among certain religious groups in the United States and Europe), all or some of the fragmented identities may take the form of possessing spirits, deities, demons, animals, or mythical figures. Acculturation or prolonged intercultural contact may shape the presentation of the other identities (e.g., identities in India may speak English exclusively and wear Western clothes). Possession-form dissociative identity disorder can be distinguished from culturally accepted possession states in that the former is involuntary, distressing, and uncontrollable; involves conflict between the individual and his or her surrounding family, social, or work milieu; and is manifested at times and in places that violate cultural or religious norms. Combined dissociative-psychosis episodes may be more common in cultural contexts with marked communal violence or oppression and limited opportunity for redress.
Sex- and Gender-Related Diagnostic Issues
Women with dissociative identity disorder predominate in adult clinical settings but not in child/adolescent clinical settings or in general population studies. Few differences in symptom profiles, clinical history, and childhood trauma history have been found in comparisons between men and women with dissociative identity disorder, except that women may have higher rates of somatization.
Association With Suicidal Thoughts or Behavior
Suicidal behavior is frequent. Over 70% of outpatients with dissociative identity disorder have attempted suicide; multiple attempts are common, and other self-injurious and high-risk behaviors are highly prevalent. Individuals with dissociative identity disorder have multiple interacting risk factors for self-destructive and/or suicidal behavior. These include cumulative, severe early- and later-life trauma; high rates of comorbid posttraumatic stress disorder (PTSD), depressive disorders, and substance use disorders; and personality disorder features. Dissociation itself is an independent risk factor for multiple suicide attempts. Greater severity of dissociative symptom scores is associated with a higher frequency of suicide attempts and nonsuicidal self-injury among individuals with dissociative disorders.
Functional Consequences of Dissociative Identity Disorder
Some children and adolescents with dissociative identity disorder may function poorly in school and in relationships. Others do well in school, experiencing it as a respite. In adults impairment varies widely, from apparently minimal (e.g., in high-functioning professionals) to profound. The symptoms of higher-functioning individuals may impair their relational, marital, family, and parenting functions more than their occupational and professional life, although the latter also may be affected. Many impaired individuals show improvement in occupational and personal functioning over time, while some individuals with dissociative identity disorder may be impaired in most activities of living and function at the level of chronic and persistent mental illness.
Differential Diagnosis
Dissociative amnesia. Both dissociative identity disorder and dissociative amnesia are characterized by gaps in the recall of everyday events, important personal information, or traumatic events that are inconsistent with ordinary forgetting. Dissociative identity disorder is distinguished from dissociative amnesia by the additional presence of identity disruption characterized by two or more distinct personality states.Depersonalization/derealization disorder. The essential feature of depersonalization/derealization disorder is persistent or recurrent episodes of depersonalization, derealization, or both. Individuals with depersonalization/derealization disorder do not experience the presence of personality/identity states with alterations of self and agency, nor do they typically report dissociative amnesia.Major depressive disorder. Most individuals with dissociative identity disorder endorse a lifelong negative posttraumatic emotional state, often with childhood onset, and their symptoms may appear to meet the criteria for a major depressive episode. Moreover, posttraumatic reactivity to times of year when trauma occurred (anniversary reactions), primarily manifesting with more despondency, distress, and suicidal ideation, may also appear to be major depressive disorder, with seasonal pattern. However, individuals with major depressive disorder or persistent depressive disorder do not experience dissociative fluctuations in self and agency and dissociative amnesia. It is important to assess if all or most identity states are experiencing the adverse mood state, since mood disorder symptoms may fluctuate because they are experienced in some identity states, but not others.Bipolar disorders. Dissociative identity disorder is commonly misdiagnosed as bipolar disorder, typically bipolar II disorder, with mixed features. The relatively rapid shifts in behavioral state in individuals with dissociative identity disorder—usually within minutes or hours—are atypical for even the most rapid-cycling individuals with bipolar disorders. These state alterations are due to rapidly shifting dissociative states and/or fluctuating posttraumatic intrusions. Sometimes these shifts are accompanied by rapid changes in levels of activation, but these usually last minutes to hours, not days, and are associated with activation of specific identity states. Elevated or depressed mood may be experienced as loculated in specific identities, through overlap/interference phenomena. Usually, the individual with dissociative identity disorder does not have a classic bipolar sleep disturbance (e.g., reduced need for sleep), instead suffering from chronic, severe nightmares and nocturnal flashbacks that interrupt sleep.Posttraumatic stress disorder. A majority of individuals with dissociative identity disorder will have symptoms that meet diagnostic criteria for comorbid PTSD. Dissociative symptoms characteristic of dissociative identity disorder should be differentiated from the dissociative amnesia, dissociative flashbacks, and depersonalization/derealization characteristic of acute stress disorder, PTSD, or the dissociative subtype of PTSD. Dissociative amnesia in PTSD typically manifests only for specific traumatic events or aspects of traumatic events, as opposed to the chronic, complex dissociative amnesia characteristic of dissociative identity disorder. Depersonalization/derealization symptoms in the dissociative subtype of PTSD are related to specific posttraumatic reminders. Depersonalization/derealization symptoms in dissociative identity disorder may occur not only in response to posttraumatic reminders, but also in an ongoing fashion in daily life, including in response to stressful interpersonal interactions and when there is overlap/interference between states.Schizophrenia and other psychotic disorders. Individuals with dissociative identity disorder may experience symptoms that can superficially appear similar to those of psychotic disorders. These include auditory hallucinations and symptoms characteristic of intrusions of personality states into the individual’s awareness; these symptoms can seemingly resemble some of the Schneiderian first-rank symptoms formerly considered indicative of schizophrenia (e.g., thought broadcasting, thought insertion, thought withdrawal, hearing voices keeping up a running commentary about the individual). For example, hearing different personality states discussing the individual can resemble auditory hallucinations of voices arguing in schizophrenia. The individual with dissociative identity disorder may also experience the thoughts or emotions of an intruding personality state, which can resemble thought insertion in schizophrenia, as well as experience the sudden disappearance of these thoughts or emotions, which can resemble thought withdrawal. Such experiences in an individual with schizophrenia are usually accompanied by delusional beliefs about the cause of those symptoms (i.e., thoughts being inserted by an outside force), whereas individuals with dissociative identity disorder typically experience these symptoms as ego-alien and frightening. Individuals with dissociative identity disorder may also report a range of visual, tactile, olfactory, gustatory, and somatic hallucinations, which are usually related to autohypnotic, posttraumatic, and dissociative factors, such as partial flashbacks, in contrast to individuals with schizophrenia, whose hallucinations are primarily auditory and less commonly visual. Dissociative identity disorder and psychotic disorders are therefore distinguished by symptoms characteristic of one of these conditions and not the other (e.g., dissociative amnesia in dissociative identity disorder and not in psychotic disorders). Finally, individuals with schizophrenia have low hypnotic capacity, whereas individuals with dissociative identity disorder have the highest hypnotic capacity among all clinical groups.Substance/medication-induced disorders. Symptoms associated with the physiological effects of a substance (e.g., blackouts) should be distinguished from dissociative amnesia in dissociative identity disorder if the substance in question is judged to be etiologically related to the memory loss.Personality disorders. Individuals with dissociative identity disorder often present identities that appear to encapsulate a variety of severe personality disorder features, suggesting a differential diagnosis of personality disorder, especially of the borderline type. Importantly, however, the individual’s longitudinal variability in personality style (attributable to inconsistency among identities) differs from the pervasive and persistent dysfunction in affect management and interpersonal relationships typical of those with personality disorders.Posttraumatic amnesia due to brain injury. Both dissociative identity disorder and traumatic brain injury (TBI) are characterized by gaps in memory. Other characteristics of TBI include loss of consciousness, disorientation and confusion, or, in more severe cases, neurological signs and symptoms. A neurocognitive disorder due to TBI manifests either immediately after brain injury occurs or immediately after the individual recovers consciousness after the injury, and persists past the acute postinjury period. The cognitive presentation of a neurocognitive disorder following TBI is variable and includes difficulties in the domains of complex attention, executive function, and learning and memory, as well as slowed speed of information processing and disturbances in social cognition. While depersonalization is not uncommon following TBI, the additional neurocognitive features noted above help distinguish it from dissociative amnesia that is part of dissociative identity disorder. Moreover, dissociative amnesia occurring in the context of dissociative identity disorder is accompanied by a marked discontinuity in sense of self and sense of agency, which are not features of TBI.Functional neurological symptom disorder (conversion disorder). Functional neurological symptom disorder may be distinguished from dissociative identity disorder by the absence of identity alteration characterized by two or more distinct personality states or an experience of possession. Dissociative amnesia in functional neurological symptom disorder is more limited and circumscribed (e.g., amnesia for a nonepileptic seizure).Factitious disorder and malingering. Individuals who feign dissociative identity disorder usually do not report the subtle symptoms of intrusion characteristic of the disorder; instead they tend to overreport media-based symptoms of the disorder, such as dramatic dissociative amnesia and melodramatic switching behaviors, while underreporting less-publicized comorbid symptoms, such as depression. Individuals who feign dissociative identity disorder tend to be relatively undisturbed by or may even seem to enjoy “having” the disorder, or may ask clinicians to “find” traumatic memories. In contrast, most individuals with genuine dissociative identity disorder are ashamed of and overwhelmed by their symptoms, deny the diagnosis, underreport their symptoms, and display minimization and avoidance of their trauma history.Individuals who feign the symptoms of dissociative identity disorder usually create limited, stereotyped alternate identities, with feigned amnesia related only to the events for which gain is sought, with apparent switching behaviors and amnesia only displayed while being observed. They may present an “all-good” identity and an “all-bad” identity in hopes of gaining exculpation for a crime.
Comorbidity
Disorders that are comorbid with dissociative identity disorder include PTSD, depressive disorders, substance-related disorders, feeding and eating disorders, obsessive-compulsive disorder, antisocial personality disorder, and other specified personality disorder with avoidant, obsessive- compulsive, or borderline personality traits. The most common forms of functional neurological symptom disorder include nonepileptic seizures, gait disturbances, and paralyses. Most commonly, nonepileptic seizures resemble grand mal seizures or complex partial seizures with temporal lobe foci; others may mimic absence or partial seizures.
Partial Dissociative Identity Disorder
Code: 6B65 | Description
Partial dissociative identity disorder is characterised by disruption of identity in which there are two or more distinct personality states (dissociative identities) associated with marked discontinuities in the sense of self and agency. Each personality state includes its own pattern of experiencing, perceiving, conceiving, and relating to self, the body, and the environment. One personality state is dominant and normally functions in daily life, but is intruded upon by one or more non-dominant personality states (dissociative intrusions). These intrusions may be cognitive, affective, perceptual, motor, or behavioural. They are experienced as interfering with the functioning of the dominant personality state and are typically aversive. The non-dominant personality states do not recurrently take executive control of the individual’s consciousness and functioning, but there may be occasional, limited and transient episodes in which a distinct personality state assumes executive control to engage in circumscribed behaviours, such as in response to extreme emotional states or during episodes of self-harm or the reenactment of traumatic memories. The symptoms are not better explained by another mental, behavioural or neurodevelopmental disorder and are not due to the direct effects of a substance or medication on the central nervous system, including withdrawal effects, and are not due to a disease of the nervous system or a sleep-wake disorder. The symptoms result in significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
Diagnostic Requirements
Essential Features:
- Disruption of identity characterized by the experience of two or more distinct personality states (dissociative identities), involving discontinuities in the sense of self and agency. Each personality state includes its own pattern of experiencing, perceiving, conceiving, and relating to self, the body, and the environment.- One personality state is dominant and functions in daily life (e.g., parenting, work), but is intruded upon by one or more non-dominant personality states (dissociative intrusions). These intrusions may be cognitive (intruding thoughts), affective (intruding affects such as fear, anger, or shame), perceptual (e.g., intruding voices fleeting visual perceptions, sensations such as being touched), motor (e.g., involuntary movements of an arm), or behavioural (e.g., an action that lacks a sense of agency or ownership). These experiences are experienced as interfering with the functioning of the dominant personality state and are typically aversive.- The non-dominant personality states do not recurrently take executive control of the individual’s consciousness and functioning to the extent that they perform in specific aspects of daily life (e.g., parenting, work). However, there may be occasional, limited and transient episodes in which a distinct personality state assumes executive control to engage in circumscribed behaviours (e.g., in response to extreme emotional states or during episodes of self-harm or the reenactment of traumatic memories).- The symptoms are not better accounted for by another mental disorder (e.g., Schizophrenia or Other Primary Psychotic Disorder).- The symptoms are not due to the effects of a substance or medication on the central nervous system, including withdrawal effects (e.g., blackouts or chaotic behaviour during substance intoxication), and are not due to a Disease of the Nervous System (e.g., complex partial seizures) or to a Sleep-Wake disorder (e.g., symptoms occur during hypnagogic or hypnopompic states).- The symptoms result in significant impairment in personal, family, social, educational, occupational or other important areas of functioning. If functioning is maintained, it is only through significant additional effort.
Additional Clinical Features:
- The dissociative intrusions attributed to non-dominant personality states by individuals with Partial Dissociative Identity Disorder are experienced internally and may not be obvious to observers. Observable identity alteration is typically indicative of Dissociative Identity Disorder.- Individuals with Partial Dissociative Identity Disorder often do not experience amnesia during episodes of dissociative intrusions. If amnesia does occur, it is usually brief and restricted to extreme emotional states or episodes of self-harm.- Partial Dissociative Identity Disorder is commonly associated with serious or chronic traumatic life events, including physical, sexual, or emotional abuse.
Boundary with Normality (Threshold):
- The presence of distinct personality states or dissociative intrusions does not always indicate the presence of a mental disorder. In certain circumstances (e.g., as experienced by ‘mediums’ or other culturally accepted spiritual practitioners) the presence of multiple personality states is not experienced as aversive and is not associated with impairment in functioning. A diagnosis of Partial Dissociative Identity Disorder should not be assigned in these cases.
Course Features:
- Partial Dissociative Identity Disorder is strongly linked to traumatic experiences, especially physical, sexual, and emotional abuse or childhood neglect. The onset of identity changes can also be triggered by removal from ongoing traumatizing circumstances, death or serious illness of the perpetrator of abuse, or by other unrelated traumatic experiences later in life.- Partial Dissociative Identity Disorder usually has a recurrent and fluctuating clinical course. Although symptoms might spontaneously reduce with age in older adults, periods of increased stress can cause recurrence of symptoms. Factors such as re-traumatization or chronically ongoing abuse tend to predict a poorer prognosis.- Partial Dissociative Identity Disorder often co-occurs with other mental disorders. In such cases, identity alternations can influence the symptom presentation of the co-occurring disorders.
Developmental Presentations:
- Disorganized attachment in childhood might put individuals at risk of developing Partial Dissociative Identity Disorder later in life.- The onset of Partial Dissociative Identity Disorder may occur at any stage of life, from early childhood to late adulthood.- Diagnosis in preadolescent children might be particularly challenging as Partial Dissociative Identity Disorder in children can manifest in a variety of ways, including conduct problems, mood and anxiety symptoms, learning difficulties, or what appear to be auditory hallucinations. Also, young children often project their dissociated identities onto toys or other objects, so that abnormalities in their identity may become detectable only as children age and their behaviours become less developmentally appropriate. Given adequate treatment, childhood cases of Partial Dissociative Identity Disorder tend to have a better prognosis than adult cases.- Early identity changes in adolescence characteristic of Partial Dissociative Identity Disorder may be mistaken for developmentally typical difficulties with emotional and behavioural regulation.- Older patients with Partial Dissociative Identity Disorder may present with what appears to be late-life paranoia, cognitive dysfunction, atypical mood, psychotic symptoms, or obsessive-compulsive symptoms.
Culture-Related Features:
- Features of Partial Dissociative Identity Disorder can be influenced by the individual’s cultural background. For example, individuals may present with dissociative symptoms of movement, behaviour, or cognition – such as non-epileptic seizures and convulsions, paralyses, or sensory loss – in sociocultural settings where such symptoms are common.- In some societies, presentations of Partial Dissociative Identity Disorder may occur after stressful exposures (e.g., recurrent parental affect dysregulation), which may or may not involve physical or sexual abuse. The tendency toward dissociative responses to stressors may be increased in cultures with less individualistic (‘bounded’) conceptions of the self or in circumstances of socioeconomic deprivation.
Sex- and/or Gender-Related Features:
- Females appear to be more likely than males to experience identity intrusions.
Boundaries with Other Disorders and Conditions (Differential Diagnosis):
-Boundary with Trance Disorder and Possession Trance Disorder: Some dissociative intrusions in Partial Dissociative Identity Disorder may resemble trance states, but Trance Disorder is not characterized by the presence of two or more distinct personality states. In Possession Trance Disorder, the individual’s normal sense of personal identity is replaced by an external ‘possessing’ identity, which is attributed to the influence of a spirit, power, deity or other spiritual entity. Behaviours or movements are experienced as being controlled by the possessing agent. Individuals who experience dissociative intrusions attributed to both internal and external entities should receive a diagnosis of Partial Dissociative Identity Disorder rather than Possession Trance Disorder.-Boundary with Dissociative Identity Disorder: In Dissociative Identity Disorder, discontinuities in agency and sense of self are marked (manifested in episodes of executive control, often including amnesia, and greater elaboration of the personality states), whereas in Partial Dissociative Identity Disorder, these discontinuities are less pronounced. In Dissociative Identity Disorder, two or more distinct personality states recurrently take executive control of the individual’s consciousness and functioning to the extent that they function in daily life or engage in relatively elaborate patterns of behaviour in specific situations. In contrast, in Partial Dissociative Identity Disorder, the non-dominant, alternate personality states do not recurrently take executive control of the individual’s consciousness and functioning to the extent that they perform in specific aspects of daily life, although there may be occasional, limited and transient episodes in which a distinct personality state assumes executive control to engage in circumscribed behaviours (e.g., in response to extreme emotional states, episodes of self-harm, or the reenactment of traumatic memories). In Partial Dissociative Identity Disorder, the non-dominant alternate personality states are not elaborated to the extent observed in Dissociative Identity Disorder. For example, they may not be oriented to the present, may have the identity of a child, or may be mostly or exclusively involved in reenacting traumatic memories. Furthermore, in Dissociative Identity Disorder there are typically (although not always) significant episodes of amnesia, which may be severe. In Partial Dissociative Identity Disorder, amnesia, if present, is usually brief and restricted to extreme emotional states or episodes of self-harm.-Boundary with other Dissociative Disorders:Partial Dissociative Identity Disorder is distinguished from other Dissociative Disorders by the presence of two or more distinct personality states. This does not occur in any other Dissociative Disorder (except Dissociative Identity Disorder, as described above). An additional Dissociative Disorder diagnosis should not be assigned based on phenomena that occur in specific relationship to intrusions by non-dominant personality states (e.g., memory loss, changes in motor or sensory functioning, experiences of depersonalization and derealization).-Boundary with Schizophrenia or Other Primary Psychotic Disorders: Individuals with Partial Dissociative Identity Disorder may report experiencing symptoms such as hearing voices or intrusive thoughts that may also occur in Schizophrenia or Other Primary Psychotic Disorders. However, individuals with Partial Dissociative Identity Disorder do not typically exhibit delusions, formal thought disorder, or negative symptoms or rapid onset and rapidly fluctuating symptoms (as in Acute and Transient Psychotic Disorder). In the absence of other symptoms supporting a diagnosis of Schizophrenia and Other Primary Psychotic Disorder, intrusive phenomena such as hearing voices may suggest the presence of dissociative personality states.-Boundary with Obsessive-Compulsive Disorder: Obsessive-Compulsive Disorder involves repetitive and persistent thoughts (e.g., of contamination), images (e.g., of violent scenes), or impulses/urges (e.g., to stab someone) that are experienced as intrusive and unwanted (obsessions) as well as repetitive behaviours, including repetitive mental acts, that the individual feels driven to perform (compulsions). However, Obsessive-Compulsive Disorder is not characterized by discontinuities in the sense of self and agency or the presence of two or more distinct personality states.-Boundary with Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder: Partial Dissociative Identity Disorder involves pervasive alterations in identity and sense of agency. In Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder, such alterations can occur but are limited to episodes of re-experiencing traumatic events (e.g., during flashbacks). If symptoms consistent with dissociative intrusions occur exclusively during such episodes in the context of Post-Traumatic Stress Disorder or Complex Post-Traumatic Stress Disorder, an additional diagnosis of Partial Dissociative Identity Disorder is not warranted.-Boundary with Personality Disorder: Personality Disorder, particularly with Borderline pattern, is characterized by persistent disturbances in sense of identity and self-direction, and often by problems with affect regulation. Personality Disorder does not involve the presence of two or more distinct personality states, but some individuals with Severe Personality Disorder exhibit transient
Other Specified Dissociative Disorder (type 1)
Diagnostic Criteria | F44.89
This category applies to presentations in which symptoms characteristic of a dissociative disorder that cause clinically significant distress or impairment in social, occupational, or other important areas of functioning predominate but do not meet the full criteria for any of the disorders in the dissociative disorders diagnostic class. The other specified dissociative disorder category is used in situations in which the clinician chooses to communicate the specific reason that the presentation does not meet the criteria for any specific dissociative disorder. This is done by recording “other specified dissociative disorder” followed by the specific reason (e.g., “dissociative trance”).Examples of presentations that can be specified using the “other specified” designation include the following:1. Chronic and recurrent syndromes of mixed dissociative symptoms: This category includes identity disturbance associated with less-than-marked discontinuities in sense of self and agency, or alterations of identity or episodes of possession in an individual who reports no dissociative amnesia.2. Identity disturbance due to prolonged and intense coercive persuasion: Individuals who have been subjected to intense coercive persuasion (e.g., brainwashing, thought reform, indoctrination while captive, torture, long-term political imprisonment, recruitment by sects/cults or by terror organizations) may present with prolonged changes in, or conscious questioning of, their identity.3. Acute dissociative reactions to stressful events: This category is for acute, transient conditions that typically last less than 1 month, and sometimes only a few hours or days. These conditions are characterized by constriction of consciousness; depersonalization; derealization; perceptual disturbances (e.g., time slowing, macropsia); microamnesias; transient stupor; and/or alterations in sensory-motor functioning (e.g., analgesia, paralysis).4. Dissociative trance: This condition is characterized by an acute narrowing or complete loss of awareness of immediate surroundings that manifests as profound unresponsiveness or insensitivity to environmental stimuli. The unresponsiveness may be accompanied by minor stereotyped behaviors (e.g., finger movements) of which the individual is unaware and/or that he or she cannot control, as well as transient paralysis or loss of consciousness. The dissociative trance is not a normal part of a broadly accepted collective cultural or religious practice.
Excerpt from News.ISST-D.org“March 5th is observed as Dissociative Identity Disorder Awareness Day in efforts to increase awareness of and education about DID.”There is not a day of awareness specific to OSDD or OSDD-1.
5th March: DID Awareness Day
23rd February: DID Pride Day
Excerpt from The Entropy System Website“Being Multiple isn't shameful. It is a sign of survival. All the alters in a system were born to help a mind survive terrible things and had to work to work together to get through it. From our perspective, that is something to celebrate! We love each member of our system and we are proud of how far we've come together. We want other systems to feel this way, too.That is why we proposed System Pride Day and the System Pride flag.”
Alter(s) and Other Terms
Summary: “Alter(s)” is one of many terms used for the separate identities within a person with DID (or OSDD/P-DID).
Everyone has parts of self. Trauma can cause barriers to be put up between these parts of self, inhibiting the ability to smoothly transition between said parts. “Alter(s)” is one term for these separate parts of self. Alters are not additional; they don’t come in from outside the brain and then leave when we heal. People without these barriers, who do not have DID or any of its variants, still have parts of self, but the parts are fully integrated- the transition between those parts of self is smooth. Despite the parts being integrated, some people may find benefit in being able to recognize and name these parts, such as in doing parts work: Internal Family Systems Therapy, Ego State Therapy, Parts Party, etc.The severity of these barriers is a spectrum and many disorders appear on this spectrum; lived experience is going to cover every possible point on that spectrum, and so the degree of separation of parts and/or how to categorize the nature of the separation may be clear in some cases and less clear in others. Excepting this, misdiagnosis, and lack of access to adequate mental health treatment, the diagnoses that involve separation to the point of alters are Dissociative Identity Disorder in the ICD-11 and DSM-5-TR, Partial Dissociative Identity Disorder in the ICD-11, and Other Specified Dissociative Disorder Subtype 1 in the DSM-5-TR.Just as a single, integrated person’s personality is influenced by their life experience, so will each alters’ be. Alters can develop their own unique personalities because alters can have different memories, different parts of the same memory, different perspectives on the same memories, and even pseudomemories.People with DID et al. often conceptualize themselves as separate people or identities within one body. How separate they feel they are depends on the individual. In order to refer to these separate identities, terms such as “alter(s)” are used. There will also be people with DID et al. that do not consider themselves separate, and who may not want to be referred to as separate.Some have no preference, some have a strong preference for or aversion to a certain term or certain terms, some prefer/use a mix of many or any terms, and some choose to use their own unique terms.Opinions may differ between individuals as there are many different possible terms to use:Excerpt from “The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization” (publ. 2006)“In the clinical literature many different constructs are used to denote what we prefer to call dissociative parts of the personality, such as ego states, dissociative or dissociated states, dissociated self-states, dissociative identity states, dissociative personality states, alter personalities or alters, dissociative or dissociated selves, dissociative identities.”
Dissociative / Part(s) / of Self
(Alternate / Alternative / Alter) State(s) of Consciousness
(Alternate / Alternative / Alter) State(s) of Identity
(Alternate / Alternative / Alter) (Identities / Identity) State(s)
(Alternate / Alternative / Alter) (Personalities / Personality) State(s)
(Alternate / Alternative / Alter) Ego(s) / State(s)
Headmate(s)
Sysmate(s) / System Mate(s)
Alt(s)
Other(s)
Self / Selves
Side(s)
Fragment(s)
Piece(s)
Facet(s)
Aspect(s)
Mode(s)
Protector(s)
Defender(s)
Mask(s)
Face(s)
Insider(s)
Voice(s)
Dialogue(s)
Role(s)
Co(llaborator)(s)
Dimension(s)
Splinter(s)
Segment(s)
Entity / EntitiesSome choose to use more casual/everyday terms:
(Person / People) (In / Of / That Share) (My / Our) (Head / Brain / Body)
(Head / Brain / Body) (Buddy / Buddies)
Guy(s)
Housemate(s)
Friend(s)
Family
Narrative(s)
Story / Stories
(Community / Crew / Team) / Member(s)
Age Cut-Off
Summary: There is a point in each person's life where their personality has integrated to a point that, even if they experience trauma, they will not develop DID/OSDD-1; there is not, and there likely won’t be, an official cut-off age for DID/OSDD-1.
Excerpt from Dr Mike Lloyd Introduces Dissociative Identity Disorder | #AskTheExperts by MultiplicityAndMe on YoutubeJess: “As well, is there a cut off point to develop DID? I've heard some people kind of say it's between, like, three and a six or a six and a nine and- yeah I'm just quite curious about when the ending is.”Dr. Mike LLoyd: “I don't think we know enough at the moment. I think the child- uh, studies on children with complex trauma and dissociation is at a very early stage. People like Renee Marks are doing the sort of the leading work on this in terms of diagnosis and therapy. The problem we've got is that ‘how do we really know?’, because so many children that are in traumatic or in abusive circumstances are not the ones that are going into health services and being picked up for help. So, the age at which a person is developing DID is likely the age at which they're undergoing the greatest level of trauma- and they're going to be hidden from health services.We don't really know- I- There is definitely a cutoff point where you could say that- let's say if you're 18 years old and you get kidnapped and tortured for a period of two years; you'll dissociate, but you're not going to develop DID. So it's the emerging pattern of the development of identity in the brain. We don't have a- what's called a critical window for the development of our identity- though ducks have a critical window, so they have to imprint within a very short space of time on to an adult in order to learn how to be a duck- that doesn't exist within the human being. We don't have that cutoff point to say that our identity is completely and utterly certain by the age of [wordless gesture]. It's just not there because there's so many infinite probabilities for how identity can be formed and at what point does personality stop developing? Is it 10? Is it 12? Is it 15? Is it 25?The- we're not really- I don't think- it's- it's almost like it's a pointless question to answer because if anyone does come up with an answer there's always going to be someone that doesn't fit into it. I think we just have to say that DID is largely a phenomenon that is generated in childhood. Whether it goes into adolescence or not I think it's still up for grabs. I think again that's a good research thing, but how do we research that in clinical trials? We definitely know that DID exists in children and Renee Marks is probably one of the world's leading therapists and clinicians in this field and she works clinically with children who have DID and she has demonstrated the DID in those kids. So [having DID is] not just an adult thing- it's an adult thing, it's a child thing, it's a teenage thing. We just have to see it as being part of human experience at this stage.”
Age of Onset
Summary: There is no age at which you become at risk for developing DID et al. because DID et al. is something (integration) that fails to happen; there is not an age that humans need to be or pass in order for trauma to become relevant.
According to “The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization” (publ. 2006), "The presence of trauma-related disorders has been linked to the age of the individual at the time of traumatization. The younger the person, the more likely a trauma-related disorder will develop."The Theory of Structural Dissociation tells us that we all begin life needing to integrate and Dissociative Identity Disorder et al. is a disruption of this developmental process due to trauma. Trauma can happen not only at birth, but also in utero / in the womb.
Blendy
Our personal word for when multiple of us are present and we have temporary blended into one being. Blue and Red have temporarily become Purple, and will very likely separate again back to Blue and Red later.
Blobby
Our personal word for when multiple of us are here all jumbled up in a ball, a bit of me here and a bit of them there and more of me over here.
Blurry
Our personal word for when multiple of us are present and our edges are blurring together, hard to know where one of us stops and the other begins.
Co-Con / Co-Conscious
The state of having two or more alter(s) occupying the conscious mind and aware of the outside world. Co-Conscious alters may or may not be able to communicate directly.(Consciousness is a spectrum of awareness, not strict lines and neat boxes.)
Co-Front / Co-Fronting
Co-front is a metaphorical (though sometimes existing in the Inner World) space that an alter resides in while they are controlling the body. To be co-front, in co-front, or co-fronting is the action of controlling the body along side another alter or alters.(Consciousness is a spectrum of awareness, not strict lines and neat boxes.)
Communication, External
When trying to communicate it is important to be patient and accepting of your alters- what they say, what they feel, how long it takes them to respond, allowing for them to not respond at all, etc. Be encouraging as well; if you’re mentally chanting “please no one show up,” they might feel like it’s better to stay hidden.Try and leave communication some where that you spend a lot of time- physically or on your phone. Multiple options for communication can be helpful.- Paper Journal
- Digital journal with Octocon (an app for pwDID) & Lighthouse (a website for pwDID)
- Videos to yourselves
- Sticky notes or notes stuck up with a magnet or tape
- Chalkboard(s) or Whiteboard(s)
- Sharpie on masking tape on pants, walls, etc
- Speak to yourselves out loud
- Play or sing music with a message and try to focus that message or the energy and imagery the song brings inward
- Voice messages
- Phone alarms/reminders
- TwiNote & Mytter apps (fake twitter for just you with your own profiles)
- Mystagram app (fake instagram for just you with you own profiles)
- Privately message your parts with each your own profiles with Antar chat app, SelfTalking app, Simply Plural (an app for pwDID) or a private server on the Discord app with PluralkitIt may be useful to put up a large sign or set a phone background that indicates the location(s) of the(se) avenue(s) of communication.There are also less direct methods of communication:
- Activity log of what you’ve been up to throughout the day
- List system rules
- Alter switch log
- Planner, calendar, or other schedule
CW | Content Warning
Similar to TW, Content Warnings are meant to warn people about possibly upsetting content such as blood, nudity, and cursing.
Diagnosis
Diagnosis, at the very least, involves review of the diagnostic criteria in the DSM-5-TR. Usually it involves more, such as the application of a test such as the MID (the Multidimensional Inventory of Dissociation), the SCID-D (the Structured Clinical Interview for Dissociative Disorders), or the DES-II (Dissociative Experiences Scale).Of these three tests two, the MID and the DES-II, are self-reported. This means evidence comes from the client (the person taking the test and being assessed). Additionally, the MID grades itself and the DES-II is a case of adding together numbers from the answers and finding an average. Having the help of a professional, if possible, is crucial- the MID even asks it be used by professionals and researchers, and the DES-II recommends further clinical evaluation (through something like the SCID-D). However, if professional help is not possible due to the country you live in or your living/financial situation, these two tools may provide some guidance. If it at all possible to get professional help, these tools may provide validation and encouragement to a client, and guidance and information to a professional.
DID Therapy Goals
Personally, I have found many therapies useful for my DID, but also sometimes harmful. I have done CBT, DBT, EMDR, somatic therapy, hypnosis and self hypnosis.There are two main categories that come up as a goal for therapy with DID. One is functional multiplicity and the other is final fusion. We believe these two options are not as different as some may think.According to the most recent theories on how DID forms, people have parts, it’s just that in a person without trauma/disordered dissociation, these parts have no barriers. A person can move smoothly between their parts without amnesia or any disruption of identity. Opposing thoughts can be weighed against each other and processed smoothly, and different “modes”/mindsets can be activated and controlled at will instead of being separated with disordered transitions.Many who feel concerned about final fusion, or fusion in general, speak about it with a sense of loss- as though the parts don’t exist anymore. However, non-disordered people have parts, just without the disorder in transition and communication of information. Many who feel concerned about functional multiplicity seem to worry that it’s incomplete to still have parts- but all people have parts. Becoming functional is about decreasing the disorder in transition and communication. Both goals amount to “have parts without disorder in their function.”Additionally, some people go through therapy with only the goal of system management. Some may want to stay here and some may do this as an avenue to one of the aforementioned therapy goals. There may be a firm idea in mind, or one might play it more by ear and follow whatever feels right as therapy evolves.
Dormancy
Dormancy is when an alter, multiple alters, or the whole system of alters becomes inactive and unreachable.
Final Fusion
Final fusion is when all of the alters within a person with DID are able to merge into one cohesive personality.
Front / Fronting
Front is a metaphorical (though sometimes existing in the Inner World) space that an alter resides in while they are controlling the body. To be front, in front, or fronting is the action of controlling the body.(Consciousness is a spectrum of awareness, not strict lines and neat boxes.)
Functional Multiplicity
Functional multiplicity is when the alters in a person with DID have lowered dissociative barriers enough to work together and be functional.
Fusion
Fusion, also known as total integration, is the result of integration, when two or more parts have healed enough to merge and become one part composed of traits of those who came before. Some even achieve final fusion.There may also be complex instances where need requires two or more parts to merge, or have a complex combination of splitting and fusing happen, where it doesn’t seem that healing happened or even seems that things got worse. This can likely be attributed to (a). that healing is not linear (b) that sometimes getting better feels worse for a while and (c). that the need for safety and the perceived way to achieve it are what ultimately shapes alters.The perception of alters in someone’s head, whether they see them or hear them or otherwise, is also a metaphor- it can be very complex. For example, what appears to be one “person” in the head can be multiple alters with dissociative barriers who share a single metaphorical body, which is a way that subsystems often present.
Integration
Integration, also known as partial integration, is the action of lowering dissociative barriers. Completing integration between multiple alters is called fusion, and total integration of all alters is called final fusion.
NPC | Non-Player / Non-Playable Character
Originating in tabletop role-playing games and commonly used in reference to video games, an NPC is a character that is part of the game and can not be controlled by the people playing the game.This term has been adopted by some people with DID to reference people in the Inner World that are not alters. NPCs are often family, pets, neighbors, and other people or animals; they help the Inner World and internal life of one or more alters feel more full.
Partner System
When someone enters into a relationship with a person with DID et al., they may or may not call that person their “partner system” as a way to indicate that their partner has DID et al. Permission should be asked first, due to comfort and safety reasons.
pw... | Person / People With ...
This acronym is primarily seen being used with health conditions. It is a prefix; It is added in front of or to the beginning of a word or acronym and means “person with” or “people with”[the following condition].This is an example of Person/People First Language.
Reorganizing
Our personal word for when an alter or alters goes through a combination of splitting and fusing.
Role(s)
An alter’s role is their job. Alters may even have multiple jobs.
Role(s), List
Roles are labels used by alters to describe their strength(s) or “job(s).” This is how we use and define our roles:
There are two common categories of roles that are very broad:
| Type | Description |
|---|---|
| Internal | Their role involves them staying inside and not fronting |
| External | Their role involves them fronting, with or without other alters |
&
| Type | … | Description |
|---|---|---|
| ANP | Apparently Normal Part | Their role involves them living daily life |
| EP | Emotional Part | Their role involves them holding traumatic events or piece of events |
| Mixed | Mixed Features Part | Their role is a combination of the two, and the split may not be equal |
The third common category of roles is based on the protective purpose that the alter formed for. They can get very specific, with some labels appearing in clinical settings but many coming from alters who made them up.
All roles are protective, even if the reasoning isn’t obvious.
| Type | Description |
|---|---|
| Host / Co-Host | Alter who lives daily life |
- Auto-Pilot
- Shell
- Mask
***
- Confrontation Protector
- Emotional Protector
- Executive Protector
- Physical Protector
- Primary Protector
- Psychological Protector
- Sexual Protector
- Social Protector
- Sleep Protector
- Verbal Protector
- Spiritual Protector
***
- Emotion Holder
- Front Holder
- Memory Holder
- Skill Holder
- Symptom Holder
- Talent Holder
- Trauma Holder
***
- Front Manager
- Memory Manager
- Mood Manager / Stabilizer / Regulator
***
- Carer / Caregiver / Caretaker
-- Cheerleader
-- Hygenist
-- Soother
***
- Watcher
-- Overseer
-- Narrator
-- Nightwatch
-- Observer
***
- Architect
- Avenger
- Bridge
- Builder
- Cartographer
- Executive
- Ferryman
- Fight Part
- Gatekeeper
- Gatherer
- Locked Part
- Medic
- Memory Keeper
- Mimic / Imposter / Impersonator
- Mood Booster
- Negotiator
- Optimist
- Pessimist
- Prosecutor
- Regressor
- Special Purpose - Special specific purpose
- Work Part
Singlet
A person with DID/OSDD-1 may refer to a person without DID/OSDD-1 as a “singleton” to signify that they have a single, integrated identity.According to most sources, such as dictionary.com, the primary definition of “singlet” is “a sleeveless athletic jersey…” but other definitions include “a single unit; an unpaired or separate item.” This follows the pattern of couplet, triplet, etc.
Singleton
A person with DID et al. may refer to a person without as a “singleton” to signify that they have a single, integrated identity.The word “singleton” has many meanings that have to do with labeling something as being single rather than part of a group.
Splitting
Splitting (in DID; there are other kinds of splitting) is the action of one alter separating further and becoming two or more alters.Lack of integration of the personality and ability to split further is due to repeated childhood trauma.Splitting happens according to the needs of the person with alters, such as physical trauma splitting an alter meant to endure, or psychological splitting an alter meant to comfort, etc.It is possible to go through a complex mixture of fusing and splitting, which we personally call adapting or reorganizing.
Switching
Switching is when an alter moves into or out of the area of consciousness that is aware of the outside world, front, co-front, or co-consciousness.(Consciousness is a spectrum of awareness, not strict lines and neat boxes.)Switches can be extremely fast (fraction of a second) or extremely slow (days, weeks, months); be covert or overt; and happen rarely or frequently.The tolerance each individual alter has to experiencing a trigger without switching will vary wildly.
Trigger
Triggers cause a switch to another part. Even when someone with PTSD gets triggered, that is an emotional part fractured off of them by trauma becoming activated. In DID/OSDD-1 there are also ANP parts to activate, as well as possibly mixed parts. This activation is what a switch is.The more complex the disorder, the more complex triggers can be. Experience can expand out of just negative triggers (triggers that cause a switch for a negative reason) into neutral and positive triggers (triggers that cause a switch for a neutral or positive reason, respectfully).
TW | Trigger Warning
Similar to CW, Trigger Warnings are meant to warn people of content that may trigger past trauma such as violence or a car crash.
Type(s)
How we use and define types in our system has to do with the presentation they identify with; appearance can have a lot of meaning.
Gender
Male
Female
Intersex
Non-Human
Changeable
Same as the body in identity and presentation
Different from the body in identity and presentation
Transgender or otherwise being non-cisgender in relation to the sex they identify with.
Age
Ageless
Older
Same Age
Younger
Misaligned (ex: 4 year old adult cat)
Doesn’t Age / Age Locked
Ages Normally
Ages Steadily, but Slow
Ages Steadily, but Fast
Ages Unsteadily
Age Slider
Age Hopper
Age Regressor
Non-Human
Animal
Shapeshifter
Hybrid
Divine
Angel
Fallen Angel
Demon
God/dess
Nephilim
Demi-God
Immortal
Dead
Ghost
Ghoul
Poltergeist
Zombie
Mummy
Skeleton
Vampire
Object
Robot
Formless
"Dissociate" and "Disassociate"
Summary: “Dissociate” and “Disassociate” share a meaning relating to multiple things being detached. “Dissociate” has an additional meaning relating to a detached feeling in the mind.
“Dissociate” is a transitive and intransitive verb, as demonstrated by Merriam-Webster.com.“Disassociate” is only a transitive verb, as demonstrated by Merriam-Webster.com. When used as transitive verbs, the two words are synonymous.“Disassociate” can only be used between two things (objects, people, etc) such as “I choose to disassociate myself(1) from her(2).” The word “dissociate” is also used in this way.
When one says “I dissociate,” referencing dissociation happening within themself, they are using “dissociate” as an intransitive verb. The word “disassociate” is not used this way.
"My" and "Our"
"My" is a possessive determiner. Possessive determiners attribute possession to someone or something.The genitive case indicates possession (among other things).
"Alters" would most likely be considered a relational noun.Excerpt from Constructing a Lexicon of Relational Nouns
“Jack has been Jill’s friend for 5 years...Relational nouns refer to an entity by virtue of how it relates to something else (Barker, 2011). In the above example, 'friend' establishes a relation between its referent, Jack, and the external entity, Jill…”So when we put all of those elements together we get the following:Excerpt from Wikipedia > Possessive determiner > Semantics"For possessive determiners as elsewhere, the genitive does not always indicate strict possession, but rather a general sense of belonging or close identification with. Consider the following examples involving relational nouns:my mother or my peopleHere, a person does not own his or her mother, but rather has a close relationship with her. The same applies to my people, which means people I am closely associated with or people I identify with."
“What is the DSM?”
The DSM is the Diagnostic and Statistical Manual of Mental Disorders. The most up-to-date version is the text revision of the fifth edition, the DSM-5-TR.The DSM is a large collection of information. That information has, unfortunately, been shaped by white colonizers and therefore colored by racism, classism, ableism, etc. It needs to be read critically, with an understanding of the stigma it contains, if it is to be of use while causing the least amount of harm. One must consider the contents for what is fact, what is opinion, and what is an opinion masquerading as a fact.It is what the United States uses in their mental healthcare system, shaping the system US citizens try to function in. Despite its flaws, for someone trying to navigate the mental healthcare system in the US, it needs to be understood and utilized, especially by those who understand that the system is flawed. Until we can change it, knowing the rules well enough to bend them helps us get as close as we can to meeting our needs- and eventually break and rebuild the rules.
How & Why I Use Obsidian (a mind mapping tool)
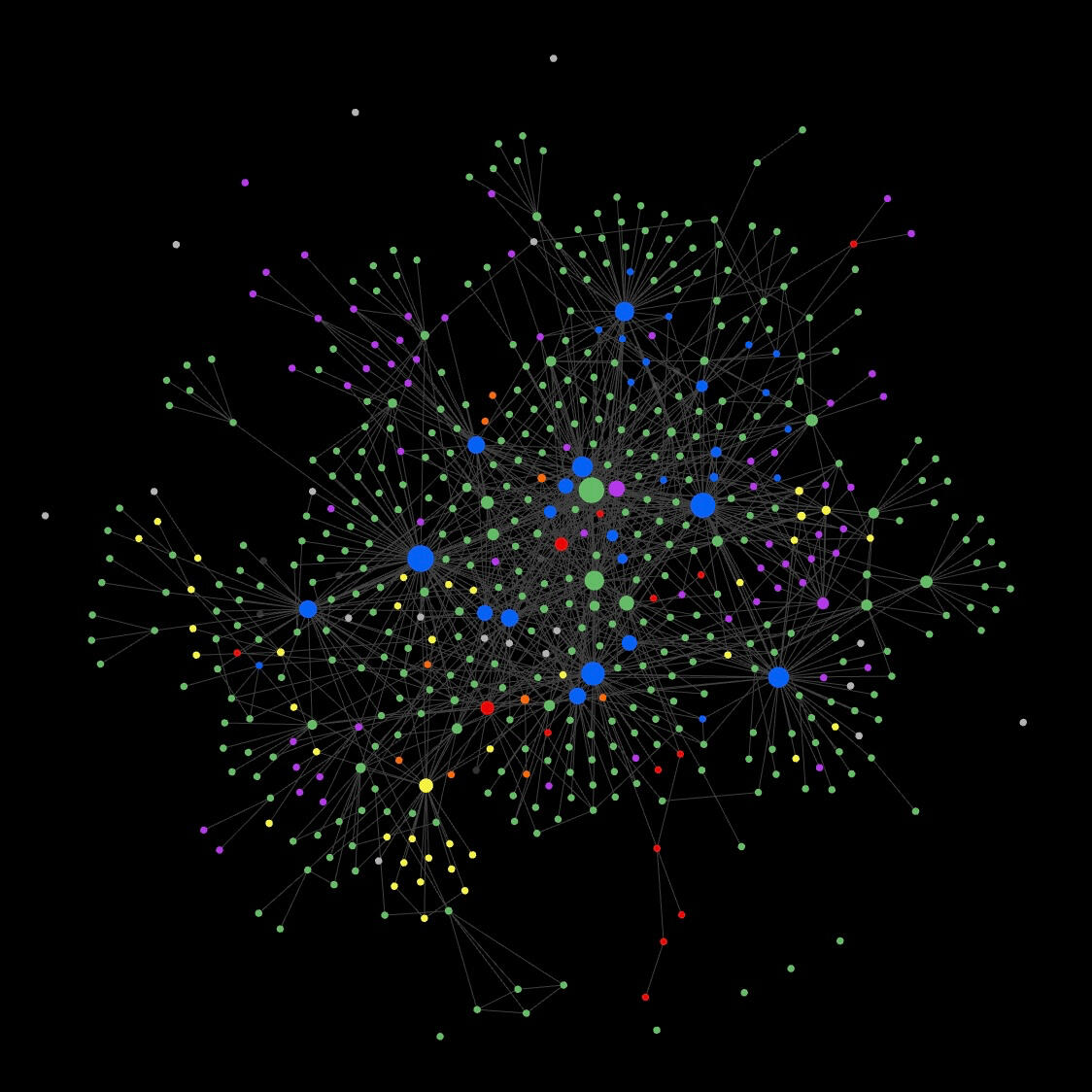
Obsidian creates a point -for each document you create- on a mind map, allows those points to be color coded from a single point by detecting a key word or symbol (as opposed to manually changing the color of each), and automatically changes the size of each point to make it bigger for each other document that leads into it.Start with all of the known conditions. List their symptoms within them, and link. Add medications and their impacts (treatment but also side effects). Add symptoms with no known cause, link those to other already-known points on the map.The idea is to create a visual representation, and map, of a person's conditions and how they relate to and impact each other.Groups:
#unknown
- Stuff that is uinvestigated; still needs to be brought up to the doctor
#wip
- Something that is in the process of being investigated; bring up to doctor
#injury
- Injuries
#attributed
- Something that has been attributed to another symptom or condition
#diagnosis
- Something that has been diagnosed
#personal
- Life impacts
100+ DID / OSDD-1 / PDID YouTube Channels
*This is not meant to be a “I agree with and recommend all of these for education because they’re perfect and unbiased” this is a “look how many we are and how long we have been around; we are not a trend, and we aren’t going away.”
Bonus Stand-Alone Videos
Have Posted Within a Year or Less
Over a Year Since Posting
150fme-aka Alicia - 2 years ago -
The A Team - 5 years ago -
Altered: A DID Podcast - 4 years ago -
ALTERnative Thoughts - 6 years ago -
ALTERSPHERE360 - 2 years ago -
Amplexus System - 3 years ago -
Angel System - 11 years ago -
Annika Rose Community - 3 years ago -
Ashlie Here - 4 years ago -
AtonalityCollective - 3 years ago -
Autistic Multiple Life - 3 years ago -
Autisystem - 4 years ago -
Bang, Broken [median system] - 5 years ago -
Blobs - 5 years ago -
Brittney Fox - 12 years ago -
CalkarianCollective - 13 years ago -
Circus System - 2 years ago -
Continuing Life System - 4 years ago -
Cracked Mirror System - 4 years ago -
Cryptid - 4 years ago -
Crystalline System - 4 years ago -
Dem System Bois - 6 years ago -
DID Explained - 3 years ago -
DIDliving - 2 years ago -
DID with me - 2 years ago -
DID/OSDD Housing - 7 years ago -
DIDiots - 3 years ago -
DIDIOTS Podcast - 3 years ago -
Dioscuri System - 5 years ago -
Dissociative Diary - 4 years ago -
Dissociative Diary - 4 years ago -
Dr. Adrian Fletcher & The Adrienne & Co. System - 2 years ago -
TheDraconicSystem - 2 years ago -
The EnchanDID System - 3 years ago -
HazyandSlightlyDazey - 2 years ago -
healing novaluna - 3 years ago -
Healing The Mosaic - 2 years ago -
IntegraDID System - 3 years ago -
John Rogers - 7 years ago -
Jon Dodge - 3 years ago -
Keegan Quill - 5 years ago -
The.Kindred. System - 3 years ago -
LifeIsMyCanvas - 5 years ago -
Lilly and Miriam - 6 years ago -
thenovembersystem - 2 years ago -
Otherbuttons & the BRB - 2 years ago -
The Patchwork Atlas System - 2 years ago -
The Phoenix System - 4 years ago -
The PolyfragmenDID System - 4 years ago -
The Sakura System - 5 years ago -
The Sour System - 2 years ago -
The System Stream - 3 years ago -
The Tangle System - 5 years ago -
Thisis DID - 6 years ago -
The Unconventional Mom - 5 years ago -
Vudu System - 6 years ago -
Zephyr Heartwell - 5 years ago -
Non-English
French
Spanish
Digital Self-Communication / Journaling Platforms
Lighthouse - Lighthouse is a website that allows a private collection of journals to be made with a list of authors that can write in them.
Simply Plural - App allows the creation of detailed profiles, including custom fields, that can be shared with friends who have a Simply Plural account (accounts for those without alters can also be made). Privacy of most areas can be customized, aside from private notes for each profile and a private group of customizable chats for all the profiles of one account to talk to each other on.
SelfTalking - App can be passcode locked and hold multiple offline chat conversations between multiple profiles that can have a custom color, name, profile picture. The profiles can be arranged in a specific order or sorted different ways, and you can customize chat background and font.
Antar chat - App can be biometric locked and and hold multiple offline chat conversations between multiple profiles that can have a custom color and name. The profiles cannot be sorted or rearranged, and the app cannot be further customized. App does contain meditative “Let It Go” feature where messages that are sent within the “Let It Go” chat disappear along with dandelion fluff.
Mytter - Fake offline Twitter with the ability to make multiple profiles.
TwiNote - Fake offline Twitter with the ability to make multiple profiles.
Mystagram - Fake offline Instagram with the ability to make multiple profiles.
Discord & Bots - Discord is an app that allows multiple group chats in one- the collection of group chats is called a server. Servers can have just the creator in them or many people, and each individual chat’s privacy can be customized or they can be organized into labeled groups. Bots are free additions that you can invite to each server that can change the name and profile picture of your sent messages.
Octocon - Octocon is an app and a Discord bot. The app communicates with its Discord bot to change the profile and name that appears for messages sent in Discord according to detailed profiles in Octocon. It also has a journal feature in the app.
Tupperbox - Discord bot that allows the creation of fake Discord accounts, changing the name and profile picture according to brackets specific to each profile/“tupper.” Profiles can also have nicknames or be organized into groups.
Pluralkit - Discord bot that allows user to change the appearance of messages, changing the name and profile picture according to a code typed at the beginning or end of a message. Profiles can be given nicknames and other biography information, and can be displayed in alphabetical order.
Other Resources
Download Obsidian, a mind mapping tool
Faces of One - tumblr comic - & Faces of One - instagram comic -
Hello World, We Exist. From System - tumblr comic -
The Patchwork Quilt: A Book for Children About Dissociative Identity Disorder - book description on Storygraph -
Not DID Specific
Ali Davis - linktree - & Pretti Graffiti Foundation Website created by Ali Davis - first and only nonprofit in the US that provides humanitarian aid for survivors of non-war related childhood torture -